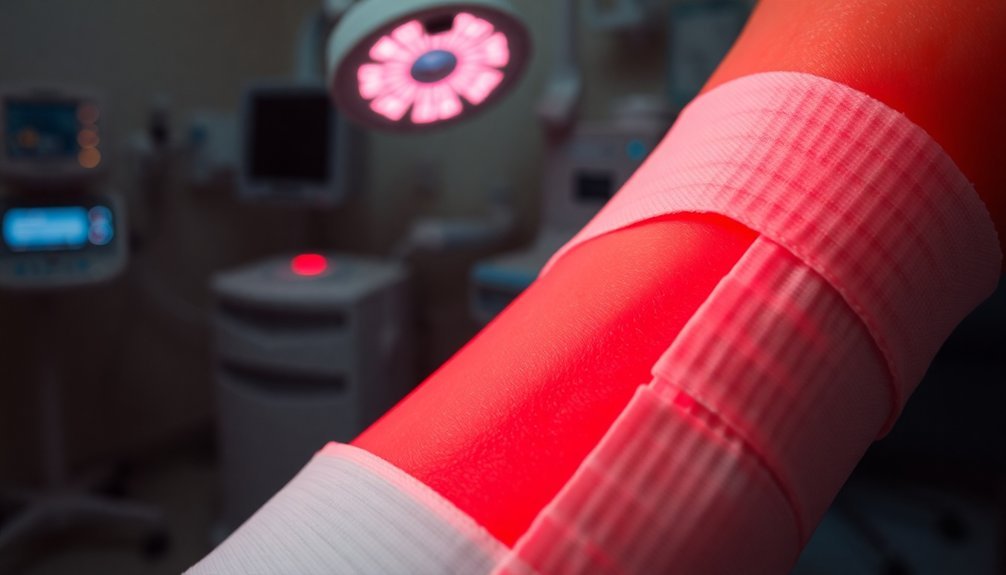
Red-LED therapy speeds up the healing of diabetic wounds by boosting cellular processes and increasing collagen production. This therapy enhances blood flow, improves nutrient delivery, and reduces inflammation, paving the way for quicker recovery. In fact, studies show that wounds treated with this therapy heal in about 21 days compared to 40-60 days for untreated ones. Plus, it effectively manages pain, making your healing journey more comfortable. Many patients report significant reductions in wound size with consistent use. If you're curious about how it works and its benefits, you'll want to explore more on this innovative approach.
Mechanism of Red Light Therapy

Red light therapy works by fundamentally enhancing cellular processes in your body, primarily through increased adenosine triphosphate (ATP) production. This boost in ATP serves as the primary energy source for your cells, enabling them to function and regenerate more efficiently.
With enhanced ATP levels, your cells experience reduced oxidative stress, allowing them to respond better to damage and rejuvenate themselves effectively. Additionally, red light therapy significantly increases collagen production, further supporting tissue regeneration and improving the overall healing process.
Beyond ATP production, red light therapy plays an essential role in reducing inflammation. It targets both acute and chronic inflammation, promoting a more favorable environment for healing.
By lowering inflammation, this therapy not only decreases pain and swelling but also accelerates the overall healing process.
Finally, red light therapy encourages tissue regeneration by stimulating fibroblast production, which is necessary for creating collagen and connective fibers.
Increased collagen synthesis strengthens your skin, while improved blood flow facilitates nutrient and oxygen delivery to wounds.
Together, these mechanisms create a healing environment that helps wounds close faster and more effectively.
Benefits of Wound Healing
When you explore the benefits of wound healing, you'll notice enhanced cellular response as a key factor. This improvement accelerates the healing process, leading to quicker recovery and less downtime. Additionally, effective pain management boosts your comfort, making the entire healing journey smoother. Maintaining a moist environment is crucial, as it significantly contributes to faster healing rates and reduces the risk of infection.
Enhanced Cellular Response
Enhanced cellular response plays an essential role in the effectiveness of wound healing, particularly for diabetic patients. With red LED phototherapy, you boost cell signaling, enhancing your cells' ability to respond to cytokine stimuli. This therapy activates G-protein receptor pathways that transmit signals crucial for healing.
You'll notice an upregulation of antiviral pathways, improving the response of genes related to immune function.
Moreover, red and green LED light facilitates improved cell migration and proliferation. The green light specifically helps diabetic cells divide and replicate, allowing them to invade and repair the wound area more effectively. This process enhances the action of M2 macrophages**, which promote tissue homeostasis and healing.
As a result, you experience enhanced cellular homeostasis and metabolism, essential for proper healing.
LED phototherapy also regulates the inflammatory response in your wounds. By modulating inflammatory cytokines, you can reduce chronic inflammation, supporting a faster recovery.
You'll see improved equilibrium levels of inflammation, which contribute considerably to the healing process.
Accelerated Healing Process
By utilizing red LED therapy, you're setting the stage for accelerated healing of diabetic wounds. This innovative technology enhances tissue repair by boosting the formation of fibroblasts, cells essential for healing. It also promotes the development of new blood vessels, greatly aiding in recovery.
When you expose your wounds to red LED light, you're not just addressing the surface; you're actively reducing inflammation, a major player in delayed healing.
Moreover, red LED therapy accelerates wound closure by pulling edges closer together, especially when you use strain-programmable bioadhesive patches. You'll notice that it excels beyond traditional dressings, providing superior strength and adhesion for various wound shapes and depths. This method reduces healing times, showing results quicker than conventional approaches.
The therapy also enhances molecular processes, activating critical pathways that regulate inflammation and improve tissue repair. With red LED light, your body receives signals that promote efficient healing, whether dealing with acute injuries or chronic conditions like diabetic ulcers.
Improved Pain Management
Effective pain management is crucial for enhancing wound healing, especially in diabetic patients. When you're facing chronic wounds, managing pain helps you focus on recovery rather than discomfort.
Pharmacological approaches like topical analgesics offer pain relief without systemic side effects, while local anesthetics can temporarily ease pain during wound care. For more considerable pain, systemic analgesics, including opioids, might be necessary but require careful selection to prevent hindering healing.
Non-pharmacological methods like cold therapy and electrical stimulation can further help reduce pain and inflammation without medication. Acupuncture also stands out as a non-invasive option to alleviate pain.
Creating personalized pain management plans is essential; these plans should tailor to your specific needs, monitor progress, and adjust strategies as needed.
Additionally, incorporating red-LED therapy—photobiomodulation—can greatly benefit pain management. This non-invasive approach not only reduces pain but also promotes healing by altering cellular processes.
Clinical Evidence of Effectiveness

When considering the clinical evidence of LED therapy's effectiveness, you'll find compelling case studies showcasing significant success in wound healing.
Comparative clinical trials reveal that this approach not only accelerates recovery but also shows promise in home-based therapy setups.
Let's explore how these findings can impact your understanding of treatment options for diabetic wounds.
Case Studies Highlighting Success
Case studies demonstrate the efficacy of red-LED therapy in treating diabetic wounds, showcasing remarkable healing results across various patient profiles.
For instance, an 84-year-old woman with leg ulcerative lesions underwent self-administered red light treatment for 30 days, 15 minutes each day. By the end of the treatment, her diabetic ulcers had dried and crusted, indicating considerable healing and pain reduction due to endorphin release.
Additionally, a clinical trial involving 30 diabetic patients with grade-I foot ulcers revealed that combining low-level laser therapy with conventional treatment led to a quicker and more substantial reduction in wound area. The group receiving the combination therapy showed increased granulation and enhanced healing processes.
Further, a study on diabetic volunteers aged 30-65 noted major improvements in wound healing indices after 12 weeks of daily home-based red and infrared LED phototherapy.
Pain and sensitivity in the wound area considerably decreased as well, confirming the therapy's effectiveness.
Comparative Clinical Trials
Clinical trials consistently highlight the effectiveness of red-LED therapy in the treatment of diabetic wounds. Studies show that LED phototherapy greatly accelerates healing by reducing the wound inflammatory process and promoting new tissue formation.
You'll be interested to know that around 75% of diabetic ulcers treated with LED therapy exhibit a wound area reduction of 30-50% within just two weeks, while control groups report less than 20%.
Moreover, wavelengths around 633 nm and 660 nm have proven particularly effective in enhancing cellular functions and reducing pro-inflammatory cytokines, leading to improved healing outcomes.
Regarding healing time, irradiated wounds often heal in about 21 days, compared to 40-60 days for those that aren't treated.
When combined with conventional treatments, LED phototherapy shows even better results, leading to a considerable reduction in wound area and increased granulation tissue.
A clinical trial reported a large effect for both infrared and red LED phototherapy, making it clear that integrating red-LED therapy can greatly improve your healing efforts for diabetic wounds.
Home-Based Therapy Outcomes
Often, patients using home-based LED therapy for diabetic wounds see marked improvements in their healing outcomes. These therapies often involve daily applications of red and infrared LED devices over a 12-week period, making it convenient for you to incorporate them into your routine.
Studies indicate that infrared LEDs may be the most effective, resulting in significant reductions in wound area and improvements in the wound healing index compared to control groups.
User compliance plays an essential role in these outcomes. When you follow the instructions correctly, placing the device at the specified distance, you can expect a reduction in pain and sensitivity in the wound area.
Changes in mean skin temperature also suggest that your wounds are healing more effectively.
Data analysis reveals a large clinical effect, particularly with infrared therapy, showing statistically significant improvements.
Follow-up assessments conducted at intervals, such as days 30, 60, and 90, help track your progress, ensuring that you're on the right path.
With the right setup and commitment, home-based LED therapy can be a game-changer in the management of diabetic wounds, offering you hope and potentially faster recovery.
Pain and Inflammation Management
Managing pain and inflammation is essential for successful wound healing, especially in diabetic patients. Red light therapy offers a powerful solution for alleviating both. It reduces pain during the healing process by promoting tissue repair and lowering the production of pain-inducing inflammatory substances.
Studies reveal that patients receiving red and near-infrared light therapy experience markedly less pain than those who don't receive the treatment. Over a 90-day period, red light therapy led to substantial pain reduction in diabetic foot ulcers.
Additionally, this therapy effectively decreases inflammation, a vital factor in preventing infections and enhancing healing. By applying low-power laser or LED light, you can effectively manage inflammation, which prevents long-lasting or recurrent inflammatory responses that could complicate healing.
Clinical trials have demonstrated that red light therapy not only enhances wound contraction and increases tensile strength but also reduces inflammatory markers in diabetic ulcers.
Ultimately, red light therapy serves as a safe, natural alternative to prescription medications and invasive procedures, minimizing the risk of side effects. By integrating this effective method, you can take meaningful strides toward pain and inflammation management, paving the way for improved healing outcomes.
Role of Microcirculation

Microcirculation plays an essential role in wound healing, as it directly impacts the delivery of nutrients and oxygen to tissues.
When you've got enhanced microcirculation, you're reducing the risk of complications, making it easier for wounds to heal effectively.
Importance of Microcirculation
Understanding the importance of microcirculation is vital for anyone dealing with diabetic wounds. In diabetic patients, microcirculation often suffers despite normal macrocirculation. This compromise leads to vascular insufficiency, making recovery challenging. Factors like decreased red blood cell deformability, increased blood viscosity, and endothelial dysfunction greatly impair microcirculatory function.
Adequate microcirculation is essential for effective wound healing since it guarantees the delivery of oxygen and nutrients to the healing tissues. When microcirculation is compromised, tissue oxygenation decreases, ultimately hindering cellular integrity and function. This insufficient oxygen level prevents fibroblasts from differentiating into myofibroblasts, which are necessary for proper wound contraction.
Additionally, reduced microcirculation negatively impacts collagen synthesis, vital for providing tensile strength and assisting in tissue remodeling.
Improving microcirculation can enhance healing outcomes in diabetic wounds. Effective therapies, like red-LED treatment, can stimulate blood flow in the wound area, supporting overall recovery. By recognizing the importance of microcirculation, you can better understand the processes affecting wound healing and explore effective treatments to optimize recovery in diabetic patients.
Enhanced Nutrient Delivery
While you may not realize it, enhanced nutrient delivery is crucial for the healing of diabetic wounds, and effective microcirculation plays a key role in this process.
When you undergo red-LED therapy, the improved blood flow greatly increases the delivery of essential nutrients and oxygen to the wound site. Measurements taken with Laser Doppler confirm that treated areas show a marked boost in microcirculation compared to those that didn't receive the therapy.
This enhanced microcirculation not only provides vital proteins, calories, and micronutrients but also aids in removing waste products that hinder healing.
Proper hydration is critical for maintaining this blood flow, ensuring that nutrients reach the cells that need them most.
Vitamins like Vitamin C contribute considerably to collagen formation and tissue repair, further supporting the healing process.
Reduced Complication Risks
Effective microcirculation plays an essential role in reducing complication risks associated with diabetic wounds. By improving blood flow, red LED therapy boosts oxygen delivery and nutrient supply to the wound area, enhancing your body's natural healing processes.
Here are some important benefits of improved microcirculation:
- Prevents Delayed Healing: Enhanced blood flow addresses endothelial dysfunction, reducing the chances of chronic wounds.
- Promotes Better Tissue Oxygenation: Increased oxygen availability is vital for effectively repairing damaged tissues.
- Stimulates Cellular Activities: Increased cell proliferation and collagen production speed up recovery and minimize complications.
- Reduces Pain and Inflammation: By alleviating pain and providing an anti-inflammatory effect, it supports a better healing environment.
This therapy not only fosters a healthier internal environment but also reduces the likelihood of serious issues like infections or amputations.
Enhancing Tissue Repair
Red and near-infrared light therapy greatly enhances tissue repair by stimulating crucial cellular processes.
You'll notice that this therapy boosts cellular energy through photobiomodulation, which improves cellular metabolism and function. As your cells proliferate, migrate, and adhere more effectively, your wound healing accelerates considerably.
The therapy also prompts the release of growth factors that activate fibroblasts, leading to increased collagen production critical for strong tissue. By modulating pain receptors, it helps reduce pain signals, making your healing more comfortable.
Additionally, it encourages improved microcirculation and blood flow, delivering essential nutrients and oxygen directly to the wound area.
You'll benefit from enhanced granulation and epithelization, resulting in new tissue rich in collagen and capillaries. This not only strengthens the skin but also alleviates associated pain and itchiness.
As red light therapy increases the activity of various immune cells, it supports your body's natural healing processes.
Fundamentally, you're not only speeding up the repair of your wounds but also enhancing your overall cellular health, making this therapy a valuable ally in your recovery journey.
Case Studies and Testimonials
Numerous case studies and patient testimonials highlight the effectiveness of red LED therapy in treating diabetic wounds. These real-life experiences emphasize the therapy's potential in accelerating healing and improving patient comfort.
Consider these compelling examples:
- An 84-year-old woman with leg ulcers experienced significant improvement after just 30 days of daily 15-minute red light treatments, with her ulcers drying and crusting.
- In a clinical trial, 30 diabetic patients treated with a combination of low-level laser therapy and conventional methods showed faster wound area reduction and increased granulation.
- A double-blind study revealed that by day 90, 58.3% of ulcers in the red light therapy group were fully healed, and 75% achieved 90-100% healing.
- Among 60 patients with chronic diabetic wounds, those receiving LED red light therapy exhibited significant advancements in wound granulation and healing.
These cases reflect the positive outcomes many face with red LED therapy, showcasing not just improved healing times but also enhanced overall well-being.
It's clear that this innovative treatment option is making a profound difference in the lives of those with diabetic wounds.
Home-Based Treatment Approaches
When managing diabetic wounds at home, utilizing red LED therapy can offer a practical and effective solution. To get started, you'll need devices designed to emit specific red and near-infrared wavelengths, such as 635 nm, 660 nm, 850 nm, and 890 nm.
For best results, hold the device about 10 cm away from the wound while treating for just 30 seconds to 5 minutes, two to three times a week.
Before each session, make sure to clean your wound with physiological saline and gauze. You can apply LED probes directly to the wound surface or use specialized insoles equipped with LED matrices and covered with latex. Securing the device with Velcro strips helps maintain proper positioning.
Don't forget to rest during treatment to optimize healing.
Monitoring your wound's progress is essential. After initiating therapy, you'll likely notice significant improvements in healing rates, lower pain, and inflammation.
Always consult your doctor before starting therapy, especially for any complex wounds. With careful application, you can enhance the healing process and increase the chances of recovery using red LED therapy right from home.
Future Research Directions

Emerging research on red LED therapy for diabetic wounds promises exciting advancements in treatment effectiveness and patient outcomes. To fully realize this potential, several future research directions should be prioritized:
- Wavelength Enhancement: Further studies should pinpoint the ideal wavelengths for different types of wounds, building on promising findings with 660 nm and 890 nm light.
- Standardized Protocols: Establishing uniform treatment guidelines based on light dosimetry, treatment duration, and frequency is essential to maximize healing potential and guarantee consistency across clinical settings.
- Patient Monitoring: Implementing thorough follow-up protocols could enhance wound healing assessment and facilitate timely interventions, ensuring wounds respond well to therapy.
- Expanding Clinical Trials: Conducting randomized controlled trials will be critical to validate the effectiveness of red LED therapy, especially in combination with traditional methods.
These directions not only pave the way for improved clinical practices but also elevate patient care, enhancing recovery rates and quality of life for those battling diabetic wounds.
Engaging in these research areas can move us closer to a future where red LED therapy becomes a staple in diabetic wound management.
Integration Into Standard Care
Frequently, integrating red LED therapy into standard diabetic wound care can revolutionize treatment approaches. By incorporating this non-invasive phototherapy, you can enhance traditional methods like antibiotics and dressings, leading to faster recovery times and decreased wound sizes.
Studies show that red and green LED therapy not only improves cell signaling and migration but also enhances ATP production, driving cellular processes essential for healing.
For best results, you should aim for a treatment schedule of three times a week for diabetic wounds, using wavelengths like 660 nm and 890 nm. Home-based interventions can be particularly effective, with daily treatments over 12 weeks demonstrating significant clinical benefits.
It's also important to monitor healing indices, including skin temperature and pain levels, to assess progress.
Clinical evidence highlights that patients undergoing LED therapy experience a reduction in wound area by 30-50%, compared to less than 20% in those receiving standard care. This improvement can also lower the risk of infections and amputations, ultimately enhancing your overall quality of life.
Embracing this innovative therapy paves the way for more effective management of diabetic wounds.
Frequently Asked Questions
How Long Does a Typical Red Light Therapy Session Last?
A typical red light therapy session lasts about 10 to 20 minutes, depending on the condition being treated. It's best to have sessions daily or multiple times a week for ideal healing results.
Are There Any Side Effects Associated With Red Light Therapy?
Yes, red light therapy can cause side effects like headaches, eye strain, and skin irritation. You should consider medication interactions and take precautions, such as wearing goggles and starting with shorter sessions to minimize risks.
Can Anyone Use Red Light Therapy for Wound Healing?
Yes, you can use red light therapy for wound healing, but it's crucial to consult a doctor first. They'll guarantee it's suitable for your specific wound type and advise on proper dosage and application.
How Often Should Red Light Therapy Be Administered for Optimal Results?
For best results, you should administer red light therapy three times a week. Some cases benefit from daily treatment, but consistency is key. Adjust frequency based on individual response for the best outcomes.
Is Red Light Therapy Safe to Use Alongside Other Medications?
Red light therapy isn't always safe with other medications. You should consult your healthcare provider to check for potential interactions, especially if you're taking photosensitizing or certain anti-cancer medications. Timing and intensity adjustments may also be necessary.
In Summary
To summarize, red LED therapy offers a promising solution for speeding up recovery in diabetic wounds. By promoting healing through enhanced microcirculation and reducing pain and inflammation, it can greatly improve your quality of life. With growing clinical evidence and successful case studies, integrating this therapy into standard care could transform how you manage diabetic wounds. As research continues to evolve, you can look forward to even more effective treatment options in the future.





Leave a Reply