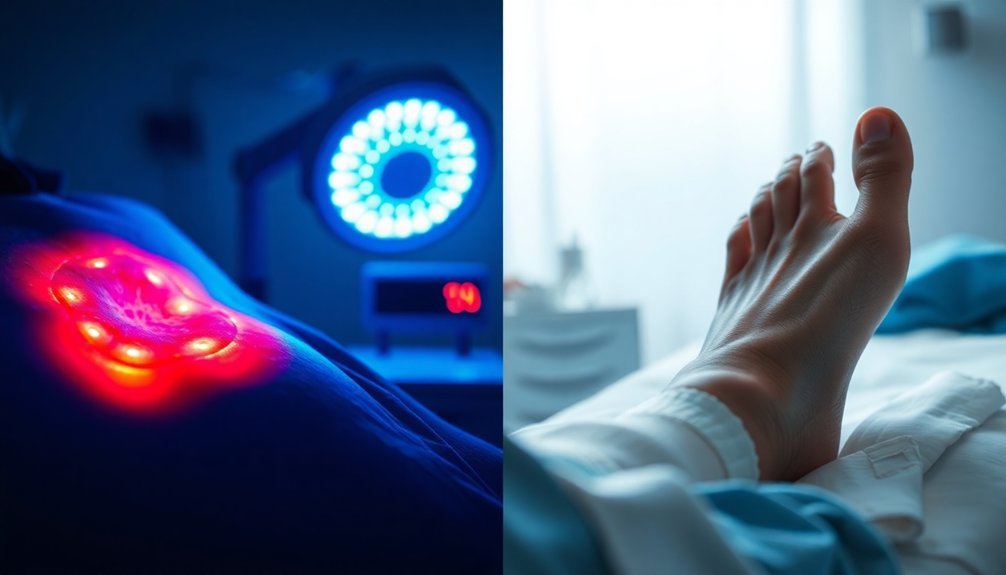
LED therapy helps diabetic wounds heal faster by boosting your body's natural healing processes. It increases mitochondrial activity, enhancing energy production and collagen synthesis, essential for wound repair. The therapy uses specific red and near-infrared wavelengths to improve blood circulation and reduce inflammation, creating a more favorable environment for healing. You'll notice that treated wounds can close markedly quicker compared to those receiving standard care. Overall, LED therapy is a safe, non-invasive option that can greatly enhance healing outcomes. If you're curious about the specifics and benefits, there's more to uncover.
Mechanisms of LED Therapy

LED therapy leverages specific wavelengths of light to stimulate cellular processes that drive healing, particularly in diabetic wounds. It boosts cellular energy by stimulating your mitochondria, which ramps up the production of adenosine triphosphate (ATP). This process enhances the energy exchange between incoming photons and key cellular components, improving your metabolic functions and increasing the viability, migration, and proliferation of diabetic wound cells.
You'll find that LED therapy greatly increases collagen production and fibroblast activity, both critical to effective wound healing. This therapy enhances the formation of granulation tissue and stimulates wound repair via heightened cell proliferation, migration, and adhesion—all without causing initial tissue damage, unlike some other laser treatments. Moreover, it reduces inflammation by decreasing free radicals in the wound bed, alleviating oxidative stress that can lead to further tissue damage. This protective effect extends to modulating pain receptors, which can help reduce discomfort in the healing process.
Plus, LED therapy supports immune system activity in the wound area, improving microcirculation essential for nutrient delivery, ultimately enhancing the overall healing process. Additionally, studies have shown that this therapy leads to a notable reduction in inflammation, further supporting the effectiveness of healing in diabetic wounds.
Effective Wavelengths for Healing
When it comes to wound healing, the choice of light wavelength plays an essential role in the effectiveness of therapy. Red light wavelengths, particularly in the range of 600-700 nm, penetrate deeply into tissues, raising core body temperature and promoting healing. Studies show that specific wavelengths like 633 nm and 660 nm greatly enhance tissue regeneration, increase blood vessel formation, and improve wound granulation. Impressively, research indicates that 58.3% of ulcers fully healed by day 90 with red light therapy.
Near-infrared wavelengths, ranging from 770-1200 nm, often work synergistically with red light to boost healing outcomes. These wavelengths enhance collagen synthesis, reduce discomfort, and promote epithelization, making them particularly effective for chronic diabetic wounds and burns. Additionally, red and green light therapies have been shown to significantly reduce inflammation and increase macrophage activity that supports tissue regeneration.
Using doses around 4.71 J/cm² produces promising results. While shorter wavelengths like blue and green light can raise wound surface temperature, they've proven less effective for healing compared to red light. Consequently, for best results, focusing on red light and near-infrared with appropriate dosage, frequency, and distance will enhance your healing process greatly.
Clinical Outcomes of Treatment

In evaluating clinical outcomes, LED therapy has shown remarkable efficacy in enhancing wound healing for diabetic patients. After just eight weeks, patients receiving LED treatment experienced a considerable reduction in their wound surface area, reaching a mean of 56% of their baseline compared to 65% in the control group.
You'll notice that wounds treated with LED phototherapy heal much faster—irradiated wounds often close in about 21 days, while untreated wounds can take 40 to 60 days. Moreover, LED therapy helps prepare the wound bed for further treatment options like skin grafts, making subsequent care more effective. Studies using the Falanga wound bed score confirm that the healing process improves considerably with LED therapy, creating a healthier environment that supports cellular repair.
Patients undergoing this therapy also see a decreased risk of complications, such as infections or the need for amputations, as LED therapy reduces inflammation and promotes a robust anti-inflammatory response. Impaired wound healing is a common issue in diabetic patients, and LED therapy specifically addresses this challenge by enhancing cellular processes essential for recovery.
With sustained improvements and reduced recurrence rates, LED therapy stands out as a reliable option for managing diabetic wounds and optimizing long-term healing success.
Biological Effects on Wounds
When you explore the biological effects of LED therapy on wounds, you'll see how it enhances cell migration and boosts collagen production.
This therapy also plays a key role in reducing inflammation, which can hinder the healing process.
Enhanced Cell Migration
Enhanced cell migration plays an essential role in the healing of diabetic wounds, as various studies have shown that LED phototherapy can notably accelerate this process. When you use red light, it boosts cell signaling and enhances responses to cytokines, which are fundamental for moving cells to the wound site. This therapy increases the expression of genes important for cell migration and proliferation, helping diabetic cells heal more effectively.
As red light stimulates the proliferation of fibrous, epidermal, and endothelial cells, it promotes quicker wound closure. The activation of specific receptors by the light improves cellular function and migration, while also increasing growth factors like FGF and EGF. These factors are critical for driving cell movement to the injury area.
You'll also find that red light reduces tissue permeability and edema, which creates a more favorable environment for healing. Studies confirm that LED therapy considerably enhances wound healing rates in diabetic models, demonstrating remarkable effects on cell migration.
The results speak for themselves; patients experience faster tissue repair and reduced wound area due to improved cellular activity facilitated by LED exposure.
Increased Collagen Production
Stimulating cellular activity through LED phototherapy, increased collagen production is vital for effective wound healing, especially in diabetic patients. LED light interacts with tissue, energizing cellular components like cytochrome-c oxidase in mitochondria, which boosts cellular metabolism significant for synthesizing collagen. As fibroblasts proliferate, collagen production ramps up, accelerating tissue restoration.
Clinical studies support the benefits of LED therapy, showing significant increases in collagen fiber and skin thickness in treated wound areas. For diabetic patients, this means reduced wound surface area, driven largely by enhanced collagen synthesis. Specific wavelengths, particularly red light (630 and 660 nm) and near-infrared light (850 and 880 nm), excel at promoting collagen deposition. Compared to blue light (460 nm), red and near-infrared wavelengths are far more effective.
Moreover, this increase in collagen not only strengthens the wound but also minimizes the risk of further tissue damage. By stimulating granulation tissue and enhancing vascular health, LED therapy supports nutrient delivery, fostering a faster, more efficient healing process.
Reduced Inflammation Effects
How can LED therapy notably reduce inflammation in diabetic wounds? This innovative treatment works by targeting specific cellular mechanisms. When you receive LED phototherapy, it decreases the release of free radicals by macrophages and neutrophils, limiting oxidative stress that prolongs inflammation.
By lessening tissue injuries, particularly in granulation tissue, LED therapy creates a more conducive environment for healing. Red and green LED light improves your inflammatory response, promoting the healing process by shortening the inflammatory phase.
It effectively reduces levels of free radicals in ischemic wounds and neuropathic ulcers, addressing one of the primary barriers to wound healing faced by diabetic patients. By minimizing oxidative stress, you promote a healthier healing environment.
Additionally, LED therapy enhances immune activity in the wound area. It improves cell migration and proliferation while boosting local circulation and microcirculation, further dampening inflammation.
Studies reveal that LED therapy notably reduces the inflammatory process, leading to better clinical outcomes for diabetic ulcers. When combined with standard treatments, patients often see remarkable improvements in both inflammation and wound healing.
Comparison With Other Treatments
When you consider treating diabetic wounds, combining LED therapy with other methods can lead to enhanced healing outcomes.
It's clear that using multiple approaches not only supports faster recovery but also improves overall treatment efficacy.
Combined Treatment Benefits
LED therapy offers significant advantages when compared to conventional treatments for diabetic wounds. It not only speeds up healing but also enhances comfort and safety, making it a truly effective option.
| Benefit | LED Therapy | Conventional Treatments |
|---|---|---|
| Treatment Duration | Reduced healing time | Slower healing rates |
| Pain & Inflammation | Minimizes pain, natural relief | Often requires pain medications |
| Wound Bed Preparation | Improves angiogenesis & perfusion | Limited impact on wound bed |
| Side Effects | Safe, non-invasive, no side effects | Possible complications, painful |
| Comfort | Painless, more comfortable | Can be uncomfortable |
With LED therapy, you're looking at decreased downtime and quicker recovery, which means fewer hospital visits. It addresses pain and inflammation effectively, allowing for a more pleasant experience. Additionally, the therapy enhances the wound bed, paving the way for successful treatments like skin grafts. Since there are no recorded side effects, it stands out as a preferable choice for long-term management of diabetic wounds, ensuring you receive the safest care possible.
Enhanced Healing Outcomes
Enhanced healing outcomes make a vital difference in managing diabetic wounds, showcasing the effectiveness of innovative therapies. With LED therapy, you'll notice faster wound closure, as studies show a 56% reduction in wound surface area after eight weeks.
Both red and green light work synergistically, speeding healing time in diabetic conditions. This therapy has demonstrated effectiveness comparable to patients with venous and pressure ulcers.
Moreover, LED therapy improves the wound bed preparation, increasing collagen production and reducing inflammation, which creates a healthier environment for healing. The Falanga wound bed score indicates that LED-treated wounds heal markedly faster than those receiving standard care.
When it comes to tissue repair, LED therapy promotes angiogenesis and boosts microcirculation, which are essential for rebuilding damaged tissue.
Unlike traditional methods, LED therapy is painless and offers results similar to or better than other treatments while being effective as a stand-alone option.
Limitations and Variability
Although LED therapy shows promise for treating diabetic wounds, several limitations and variabilities can affect its effectiveness. First, there's a shortage of robust studies, with only eight articles reviewed. This small number doesn't provide a strong evidence base.
Additionally, you might notice that study parameters vary widely—different wavelengths, dosages, and treatment durations all yield inconsistent results. Standardized protocols are lacking, which is essential for establishing effective treatment guidelines for diabetic patients.
Comorbidities like neuropathy and arterial diseases can further complicate outcomes. You may also find that while some patients respond well to LED therapy, others don't see significant improvements, and the reasons for this non-responsiveness remain unclear.
Furthermore, the diversity in treatment parameters—like energy intensity, application frequency, and distance from the wound—can lead to variable efficacy. The methods of evaluating healing differ across studies, contributing to confusion in results.
Finally, technical issues can arise when trying to measure physiological changes during high-energy treatment, impacting overall assessment. These factors indicate that while LED therapy holds potential, its current application needs careful consideration.
Future Research Directions

To overcome the limitations identified in current LED therapy studies for diabetic wounds, future research needs to focus on establishing standardized treatment protocols.
You'll want to see healthcare professionals, particularly nurses, develop specific guidelines based on solid scientific evidence. Evaluating the physical and clinical characteristics of ulcers alongside LED parameters could optimize healing outcomes considerably.
Furthermore, integrating LED phototherapy with other treatment methods may enhance the overall healing process.
Expanding clinical trials is vital, too. A larger pool of participants and diverse populations will strengthen the evidence supporting LED's efficacy.
You should encourage studies investigating various wavelengths and their specific effects on wound healing, while also comparing LED phototherapy to other methods like laser therapy.
Additionally, examining the mechanisms and biological effects of LED therapy is essential. Understanding how it interacts with cellular functions, reduces oxidative stress, and influences gene expression could reveal innovative treatment possibilities.
Finally, evaluating the practicality of LED therapy in diverse clinical settings and monitoring long-term outcomes can solidify its role in diabetic wound management.
Frequently Asked Questions
How Long Does Each LED Therapy Session Last?
Each LED therapy session lasts about 20 minutes. You can schedule these sessions up to three times a week, depending on your treatment plan and specific needs. Consistency is key to achieving ideal results.
Are There Any Side Effects of LED Therapy?
You won't experience significant side effects from LED therapy. It's safe, non-invasive, and typically painless. Regular treatments lead to improvement, and studies show no adverse reactions compared to control groups. Enjoy its benefits worry-free!
Can LED Therapy Be Used for Other Types of Wounds?
Yes, you can use LED therapy for other wounds, including chronic ulcers and acne. It promotes healing by reducing inflammation, stimulating new blood vessel growth, and enhancing cellular functions, helping various skin conditions effectively.
How Many Sessions Are Typically Required for Effective Treatment?
Typically, you'll need multiple sessions for effective treatment, often around three times a week for about eight weeks. The total can vary based on factors like wound severity and your response to the therapy.
Is LED Therapy Suitable for All Diabetes Types?
Yes, LED therapy's suitable for all diabetes types. It effectively improves wound healing processes by enhancing collagen production and reducing inflammation, benefiting both Type 1 and Type 2 diabetes patients with chronic wounds or diabetic ulcers.
In Summary
To sum up, LED therapy shows great promise in treating diabetic wounds by enhancing healing mechanisms and promoting tissue regeneration. Its specific wavelengths can effectively target the biological processes involved in wound recovery. While there are limitations and variability in outcomes, the potential benefits make it a valuable option in your treatment plan. As research continues to evolve, you can look forward to more refined techniques and improved results in managing diabetic wounds effectively.





Leave a Reply