Deep-tissue beam therapy works by combining two powerful cancer-fighting mechanisms. First, protons from a particle accelerator travel to a precise depth and release their energy directly at the tumor site, disrupting cancer cells' DNA while sparing healthy tissue. Second, thermal therapy heats the tumor area to 104-110°F, making cancer cells more vulnerable to treatment. You'll see success rates up to 83% for one-year survival, with fewer side effects than traditional radiation. This dual approach particularly helps with hard-to-reach cancers in your abdomen and pelvis. The fascinating details of this precision technology reveal even more impressive benefits.
The Science Behind Beam Therapy
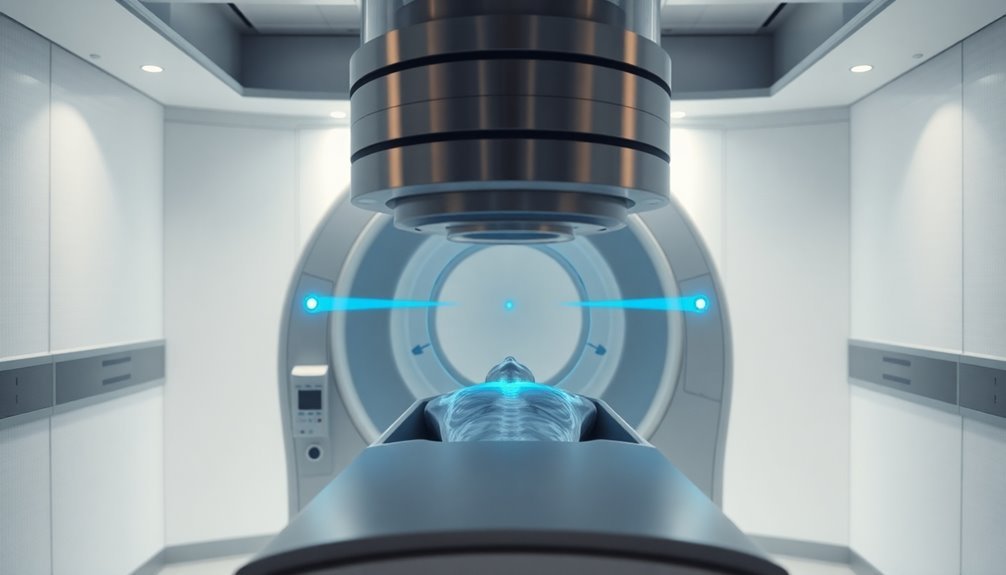
Through remarkable advances in medical technology, proton beam therapy has emerged as a groundbreaking cancer treatment that delivers precise, targeted radiation to tumor cells. You'll find that this innovative treatment uses accelerated protons to disrupt cancer cells' DNA, effectively destroying them while minimizing damage to surrounding healthy tissue.
What makes proton therapy particularly effective is its unique Bragg peak characteristic. When protons enter your body, they travel to a specific depth and release most of their energy at the tumor site before stopping completely. Most patients receive daily treatments for several weeks to achieve optimal results.
This precise control allows doctors to adjust the beam's energy based on your tumor's depth, ensuring ideal treatment delivery.
The technical process involves a particle accelerator that propels protons through a sophisticated gantry system. Using powerful magnets, the beam can be focused to as narrow as 5 millimeters, offering unprecedented accuracy in targeting tumors.
You'll benefit from this precision, especially if your tumor is located near sensitive organs like the brain, eyes, or reproductive system. This approach substantially reduces your risk of secondary cancers and minimizes side effects compared to traditional radiation therapy, making it particularly valuable for pediatric patients who need to avoid long-term radiation exposure.
Precision Targeting in Action
Modern precision targeting brings proton therapy's theoretical advantages into real-world clinical practice. You'll find two leading technologies at the forefront: MR-Linac systems and proton beam therapy.
MR-Linac combines real-time MRI tracking with precision radiation delivery, allowing your medical team to monitor tumor position continuously and adjust the beam instantly when needed. Since tumors can shift up to 20 millimeters during breathing, this tracking capability is crucial.
When you're receiving proton therapy, you'll benefit from its unique Bragg peak characteristic, where radiation stops precisely at the tumor site without an exit dose. This means you're getting maximum tumor impact while surrounding healthy tissues receive minimal exposure.
The technology's pencil beam scanning delivers radiation with millimeter accuracy, reducing your risk of secondary cancers by 26-39% compared to conventional treatments.
You'll see these precision benefits particularly in challenging cases, such as abdominal or thoracic tumors. If you're a pediatric patient, you'll especially benefit from these targeting methods, as they substantially reduce long-term radiation exposure risks.
Your treatment plan won't be static either – both technologies allow for adaptive therapy, meaning your medical team can adjust your treatment based on daily imaging and anatomical changes.
Proton Power Versus Cancer Cells
Recent clinical data reveals proton therapy's powerful impact against cancer cells, matching traditional radiation's effectiveness while substantially reducing side effects. You'll find similar survival rates between the two treatments, with proton therapy showing an 83% one-year survival rate compared to 81% for traditional X-ray radiation.
What sets proton therapy apart is its remarkable safety profile. You're markedly less likely to experience severe side effects – only 11.5% of patients face complications within 90 days, compared to 27.6% with traditional radiation. This improvement comes from proton therapy's ability to target tumors with submillimeter precision while sparing healthy tissue. The therapy achieves this through its unique Bragg peak delivery, which concentrates the highest radiation dose directly at the tumor site.
| Outcome Measure | Proton Therapy | Traditional Radiation |
|---|---|---|
| 1-Year Survival | 83% | 81% |
| 3-Year Cancer-Free | 46% | 49% |
| 3-Year Survival | 56% | 58% |
| Severe Side Effects | 11.5% | 27.6% |
The treatment's growing adoption reflects its effectiveness, with patient numbers rising from 5,377 in 2012 to 15,829 in 2021. You'll find it's now used for various cancers, including breast, GI tract, and head and neck tumors, offering a noninvasive option with minimal side effects.
Treatment Planning and Delivery
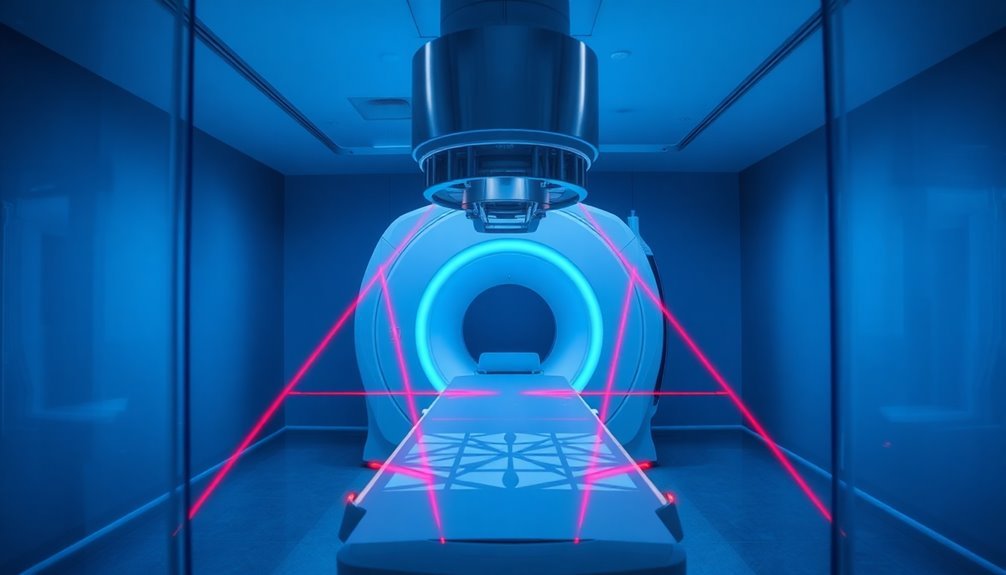
While proton therapy's effectiveness is clear, its success hinges on meticulous treatment planning and precise delivery methods. Before your treatment begins, you'll undergo a simulation process where your body is carefully measured and marked to guarantee pinpoint accuracy.
Medical teams use advanced software to create your custom plan, maximizing cancer cell destruction while protecting healthy tissue. Oral or intravenous contrast may be administered during imaging to enhance visibility of specific areas.
Your treatment plan involves several key components that work together:
- CT scans and MRIs map out the exact treatment area
- Custom body molds or mesh masks guarantee consistent positioning
- Quality assurance checks verify the plan's accuracy
You'll typically receive treatments Monday through Friday, with each session lasting about an hour. While the actual radiation delivery takes only minutes, proper setup is vital for success.
Your medical team will use imaging techniques to position you precisely before each treatment, whether you're receiving external beam radiation, proton therapy, or brachytherapy. The type of radiation and delivery method they've chosen for you depends on your specific cancer type, location, and treatment goals.
Throughout your treatment course, physicists and dosimetrists continuously monitor and verify that you're receiving exactly the prescribed dose.
Heat Enhancement and Results

Heat therapy revolutionizes the effectiveness of beam treatments by enhancing tissue response and accelerating healing processes. When you undergo deep-tissue beam therapy, the controlled application of heat triggers essential biological responses in your body.
The heat causes your blood vessels to dilate, increasing blood flow and oxygen delivery to the targeted treatment areas. The enzymatic activity increases as tissue temperatures rise.
You'll experience multiple therapeutic benefits as the heat penetrates your tissues. The increased temperature reduces your nerve sensitivity and relaxes your muscles by decreasing gamma efferent activity.
Your tissue's metabolic rate speeds up, and you'll notice improved extensibility, making recovery more efficient. The heat also stimulates your cutaneous thermoreceptors, releasing bradykinin that further enhances blood flow.
The results you can expect include faster healing times and reduced pain levels. Your tissues become more responsive to treatment as the heat increases the activity of healing enzymes like collagenase.
While you'll need professional guidance to guarantee safe application, the therapy's effectiveness is well-documented across various conditions. The combination of deep heating techniques with precise beam delivery provides you with targeted, efficient treatment outcomes.
Frequently Asked Questions
How Long Does Each Treatment Session Typically Last?
Your treatment session typically lasts 10-40 minutes, though actual radiation therapy only takes a few minutes. Most time's spent on setup and positioning. You'll usually receive treatments five days weekly for several weeks.
Can Patients Drive Themselves Home After Beam Therapy Treatments?
Yes, you can drive yourself home after proton beam therapy treatments since adults don't require anesthesia. As long as you haven't received sedation, you're free to transport yourself to and from appointments safely.
Do Insurance Companies Usually Cover Deep-Tissue Beam Therapy?
Yes, your insurance will likely cover deep-tissue beam therapy if it's medically necessary. You'll need pre-authorization, and coverage varies by plan. Medicare and most private insurers include it for approved conditions.
What Dietary Restrictions Should Patients Follow During Treatment?
You'll need to eat soft, protein-rich foods while avoiding raw produce and spicy items. Focus on small, frequent meals, stay hydrated, and choose calorie-dense foods to maintain your strength during treatment.
When Can Patients Resume Normal Exercise After Starting Treatments?
You can usually resume normal activities right after proton therapy treatments, but you'll need to follow your doctor's specific guidelines. Your recovery timeline depends on your cancer type and treatment location.
In Summary
You'll find deep-tissue beam therapy works through precise energy delivery that targets cancer cells while minimizing damage to healthy tissue. Whether you're receiving proton or photon therapy, the beams concentrate their power exactly where you need it, causing tumor cell death through direct DNA damage and heat effects. With modern treatment planning and delivery systems, you're getting highly effective, focused cancer treatment that's becoming more refined every year.




Leave a Reply