Therapy rays offer five powerful ways to eliminate dangerous wound bacteria. You'll find UVC light disrupting bacterial DNA to prevent replication, while blue light destroys cell membranes and enhances antibiotic effectiveness. Red and near-infrared light boost your body's natural healing response by reducing inflammation and increasing collagen production. Violet light helps detect hidden bacteria through fluorescence imaging, ensuring precise treatment. Finally, these rays work together to create a thorough approach that prevents bacterial resistance. The science behind these breakthrough technologies reveals an exciting new frontier in wound care.
Understanding Therapy Ray Technology

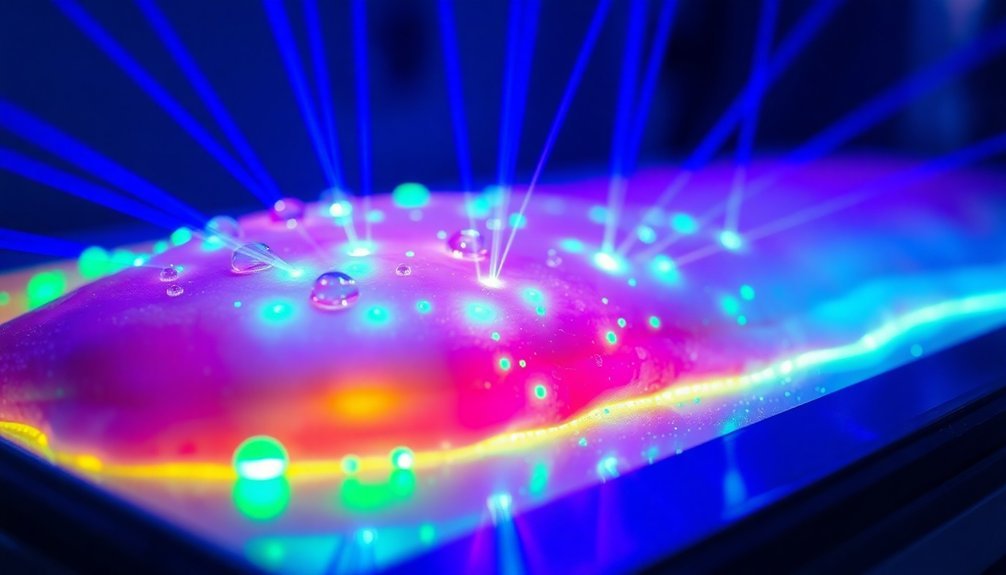
A beam of healing light represents modern medicine's innovative approach to fighting wound infections. You'll find several types of therapeutic rays being used today, each working through distinct mechanisms to combat bacteria and promote healing.
When you're dealing with UVC light therapy, it targets bacteria by damaging their genetic material, specifically in the 250-270 nm wavelength range. This process prevents bacterial replication by causing thymine molecules in their DNA to bind together.
You can expect a remarkable 99.9% kill rate against resistant bacteria like MRSA with just 5-120 seconds of exposure. Recent studies show that antimicrobial blue light has demonstrated effectiveness against multiple drug-resistant pathogens without developing resistance.
If you're looking at photobiomodulation therapy, you'll see it uses red to near-infrared light (630-1000 nm) to enhance healing. It's working at the cellular level to boost metabolism and increase collagen production.
You'll find it particularly effective when combined with other treatments for chronic wounds.
These technologies aren't just theoretical – they're practical tools in modern wound care. You'll need specific protocols, like UVC exposure for 60-180 seconds, 2-5 times weekly, depending on your wound size and type of infection.
Blue Light Against Drug Resistance
Beyond UVC and red light therapies, blue light has emerged as a powerful weapon against drug-resistant bacteria. When you're dealing with antibiotic-resistant infections like MRSA, blue light therapy offers a unique advantage because bacteria can't develop resistance against it. The light works by targeting specific molecules within bacteria, causing membrane damage and cell death without harming your healthy tissue. This innovative treatment helps address the 2.8 million antibiotic-resistant infections that occur annually in the US.
What makes blue light particularly effective is its ability to work alongside traditional antibiotics. Studies show that when you combine blue light with antibiotics, you'll get enhanced bacterial elimination, making it easier to treat stubborn infections that wouldn't respond to antibiotics alone.
- Low-intensity, continuous exposure to blue light effectively kills bacteria while maintaining safety for your skin
- The therapy targets bacterial chromophores, creating toxic effects that destroy harmful microorganisms
- Blue light increases bacteria's susceptibility to antibiotics, making previously resistant strains treatable
- The treatment promotes wound healing by both eliminating infection and reducing inflammation
For challenging wound infections, blue light therapy isn't just an alternative – it's becoming a crucial tool in modern medicine's fight against drug-resistant bacteria.
Safety Profile Of Light Treatment

Light-bathing therapy stands out for its exceptional safety profile in wound treatment. When you're using this approach, you'll benefit from low irradiance levels around 5 mW/cm^2, which effectively fights bacteria while minimizing risks to your tissue.
The continuous, gentle exposure guarantees you're getting antimicrobial benefits without the thermal damage often associated with high-intensity light treatments. The therapy's cell multiplication effects help repair damaged tissues while maintaining optimal safety levels.
You'll find that the therapy's thermal safety is particularly significant. The low-energy delivery prevents overheating of your wound bed, making it safe for extended periods of use. Whether you're dealing with sensitive areas or chronic wounds, the light-bathing approach won't cause thermal complications that could impair healing.
The biocompatibility of this treatment adds another layer of safety. You can wear light-emitting patches directly on your wound surface, as they're made with materials that won't harm your tissue. They'll work seamlessly with your existing wound dressings and treatments.
Clinical evidence backs these safety claims, with studies on rat models showing no adverse effects on wound tissues while effectively reducing bacterial presence. You're getting a non-invasive treatment that fights infection without compromising your healing process.
Early Detection Through Light
You'll find that violet light acts as a powerful tool for exposing harmful bacteria in wounds, with specialized devices able to spot infections up to 1.5mm beneath the surface.
Different bacterial species emit distinct signals when exposed to specific wavelengths, such as *S. aureus* responding to 685 nm light while both *S. aureus* and *P. aeruginosa* react to 410 nm wavelengths.
This instant detection system lets you identify the type of infection present, making it easier to start the right treatment quickly. Research shows daily light therapy successfully reduces bacterial counts in infected wounds, as demonstrated in diabetic rat studies.
Violet Light Reveals Pathogens
The detection of bacteria through violet light has emerged as a groundbreaking method in wound care. This innovative technology uses handheld devices that emit violet light, which makes bacterial cell walls visible through autofluorescence imaging. This method identifies harmful bacteria that you'd typically miss through traditional clinical assessments in about 90% of cases.
When you're dealing with chronic wounds like diabetic foot ulcers or venous leg ulcers, this technology proves invaluable. The light penetrates up to 1.5mm deep, revealing bacterial presence in real-time during wound debridement procedures. The device's fluorescence-guided approach has demonstrated sensitivity up to 400% higher than standard assessment methods. You won't need to wait for lab results to make informed decisions about treatment.
Here's what makes violet light detection so effective:
- It provides immediate identification and quantification of bacterial presence
- You can target specific areas during wound debridement with greater precision
- You'll get accurate measurements of wound areas using calibration stickers
- It helps reduce the need for prolonged antibiotic treatments
This technology's already being used in medical centers, and it's showing promise in preventing complications that could lead to amputations. You'll notice that it's particularly useful when treating various wound types, though its effectiveness may be limited in heavily calloused skin.
Instant Bacterial Detection System
Building on violet light's detection capabilities, modern bacterial detection systems now incorporate multiple light-based technologies for thorough wound monitoring. You'll find these systems can detect harmful bacteria that traditional clinical assessments often miss, with a success rate of identifying pathogens in 90% of previously undetected cases.
High-calibration LED technology, like the Bactiscan, merges four distinct wavelengths to create a green glow when detecting bacterial protein shells. These systems are particularly effective in detecting bacteria since they can examine large surface areas instantaneously. You'll appreciate how this non-destructive method instantly scans large areas for biofilms and contamination.
The UV-A light technology in devices like the BioDtex UV Lamp helps you spot dangerous microorganisms such as Listeria and E.coli on surfaces immediately.
For more precise diagnosis, you can turn to Polarization Anisotropy Diagnostics (PAD), which examines bacterial RNA sequences. You'll get results within hours through a smartphone app, making it more efficient than traditional culture tests.
These detection systems don't just identify bacteria – they're helping you prevent antibiotic resistance by enabling targeted treatments and faster interventions, ultimately improving wound care outcomes.
Different Bacteria, Different Signals
Modern light-based detection methods illuminate a fascinating truth: each bacterial species emits distinct optical signals when exposed to specific wavelengths of light. You can detect these unique signatures through various light-based techniques, including autofluorescence imaging and metal nanohybrid structures that reflect different colors based on their composition.
When you're dealing with wound infections, you'll find that autofluorescence imaging is particularly effective, successfully identifying bacteria in 9 out of 10 cases. This real-time detection method offers substantial advantages over traditional laboratory testing, helping you make faster treatment decisions. The detection process takes just one hour to complete, making it significantly faster than conventional methods that require up to 48 hours.
Here's what makes light-based bacterial detection so powerful:
- Different bacteria produce unique fluorescent signals under specific light conditions, allowing for precise identification
- Metal nanohybrid structures containing gold, silver, or copper create distinct color reflections for different bacterial types
- Optical methods can detect bacteria through reflection, refraction, scattering, or absorption of light
- Light-based detection reduces your need for antibiotics and helps prevent infection progression
This technology proves especially valuable when you're managing chronic wounds like diabetic foot ulcers, where early detection can markedly improve treatment outcomes.
Applications In Wound Care

Three major applications of therapeutic radiation in wound care have revolutionized treatment outcomes.
First, you'll find that hyperbaric oxygen therapy (HBOT) directly addresses radiation-damaged blood vessels by saturating your blood with 100% oxygen in a pressurized chamber. This helps overcome the reduced oxygen delivery that often persists even 20 years after radiation therapy. The treatment is especially crucial since both healthy and cancerous cells are affected during radiation therapy.
Second, you can benefit from MIST ultrasound therapy, which has proven particularly effective when combined with standard wound care. If you're dealing with chronic wounds or areas with low transcutaneous oxygen pressure, this treatment substantially reduces wound area and volume while accelerating the healing process.
Finally, you'll discover that specialized wound care protocols target specific radiation injuries like osteoradionecrosis (ORN) and soft tissue radionecrosis (STRN). When you're dealing with these conditions, your healthcare provider may combine HBOT with other treatments to prevent tissue breakdown. Medicare coverage for HBOT makes this treatment more accessible, especially if you're facing chronic wounds that haven't responded to standard care.
These applications work together to improve healing rates and promote better outcomes in radiation-affected tissues.
Proven Clinical Success Stories
Recent hospital trials reveal remarkable breakthroughs in therapy ray treatments, with blue light therapy achieving near-complete bacterial eradication within 44 hours.
You'll find compelling evidence in diabetic ulcer cases, where autofluorescence imaging detects harmful bacteria in 90% of cases that doctors would otherwise miss during standard examinations.
The data shows consistently infection-free healing stories, particularly when combining laser therapy with gold nanoparticles to break down resistant bacterial biofilms, leading to faster recovery times and reduced hospital stays.
Hospital Trial Breakthrough Results
Groundbreaking clinical trials have demonstrated remarkable success in preventing wound bacteria through innovative therapy techniques. You'll find that peceleganan spray showed promising results, achieving a 90.4% clinical efficacy rate by day 8, outperforming traditional silver sulfadiazine cream treatments in wound infection management.
The real game-changer is autofluorescence imaging, which detects harmful bacteria that you'd typically miss with conventional assessments. This technology's ability to identify bacteria in previously undetected cases has revolutionized wound care protocols in hospitals.
Here's what the latest hospital trials reveal:
- Negative Pressure Wound Therapy with Instillation (NPWTi) demonstrates superior bacterial reduction compared to standard NPWT, particularly between days 2 and 8 post-operation.
- Autofluorescence imaging enables real-time medical decisions, reducing unnecessary antibiotic use and helping prevent resistance.
- Peceleganan spray treatments achieve higher clinical efficacy rates than traditional methods, with similar safety profiles.
- Combined therapy approaches, integrating multiple treatment modalities, show enhanced outcomes in bacterial prevention and wound healing.
These breakthrough results are transforming how medical professionals approach wound care, offering more effective and targeted treatment options for patients with infected wounds.
Diabetic Ulcer Recovery Rates
Building on these innovative treatment methods, diabetic ulcer recovery shows remarkable progress when patients receive early specialist care.
You'll see markedly better healing rates if you seek treatment within 52 days of ulcer onset, while waiting longer can decrease your chances of recovery by 58%.
When you're facing a diabetic foot ulcer, severity plays a vital role in your recovery timeline. High-severity ulcers (grade 2/3, stage C/D) require more aggressive treatment, and you'll need urgent surgical consultation if you develop severe infections, gangrene, or deep abscesses.
For moderate to severe infections, you'll benefit from early surgery combined with antibiotics.
You'll experience the best outcomes through an interdisciplinary approach, which achieves impressive healing rates of 50.7% at three months and 77.9% at one year.
Your treatment plan will likely include dead tissue removal, wound cleaning, and proper dressing. While you'll need antibiotics for infected ulcers, they're not necessary for uninfected wounds.
To prevent future ulcers, you'll want to maintain daily foot care routines, including washing, drying between toes, and wearing appropriate footwear.
Regular checkups with your healthcare provider guarantee early detection and prompt treatment.
Infection-Free Healing Stories
Remarkable success stories emerge from patients treated with innovative therapy rays for wound infections. At Keck Medicine of USC, patients with stubborn diabetic foot ulcers have experienced dramatic turnarounds using violet light detection combined with blue light therapy.
These advanced treatments are particularly effective when traditional methods haven't worked, as they target bacteria that standard assessments often miss.
- At USC's wound care center, doctors have documented cases where autofluorescence imaging helped them identify hidden bacterial colonies in 9 out of 10 patients, leading to more precise debridement and faster healing.
- Patients receiving low-irradiance blue light therapy have shown significant bacterial reduction without the tissue damage risks associated with high-intensity treatments.
- Long-term success stories demonstrate how continuous light-bathing strategies keep bacterial biofilms from reforming, allowing natural healing to progress.
- Clinical cases reveal that combining early detection through violet light with targeted blue light therapy has helped patients avoid extended antibiotic use, reducing their risk of developing drug-resistant infections.
These documented successes show how therapy rays are transforming chronic wound care, offering hope to those struggling with persistent infections.
Transforming Traditional Wound Management
Light-based innovations are revolutionizing wound care by addressing the limitations of traditional management methods.
While conventional approaches often miss hidden bacteria and require time-consuming lab tests, new light therapies can detect and treat infections immediately. These advanced techniques help you avoid the delays that traditionally let infections worsen while waiting for test results.
When you're dealing with wound care, you'll notice that blue light therapy at 5 mW/cm² effectively prevents bacterial growth without causing tissue damage. This therapy works by targeting bacteria's natural chromophores, maintaining wound bioburden below clinically acceptable levels.
You can combine this approach with autofluorescence imaging, which uses violet light to spot bacteria that standard clinical assessments might miss.
These light-based methods integrate smoothly with existing wound care strategies, including the TIME principle and advanced dressings. They're particularly valuable because they reduce your need for aggressive debridement and excessive antibiotic use.
Future Wound Healing Breakthroughs
Standing at the forefront of medical innovation, future wound healing breakthroughs combine artificial intelligence, smart materials, and regenerative medicine to transform patient care.
You'll soon see smart bandages that can communicate with your smartphone, delivering precise drug dosages while monitoring healing progress in real-time. Advanced biomaterials will mimic your body's natural healing environment, using hydrogels and nanomaterials to reduce scarring and fight infection more effectively.
The integration of AI with electronic health records will revolutionize how healthcare providers track and treat your wounds. These systems won't just store data – they'll predict healing outcomes and suggest personalized treatment plans based on exhaustive analysis.
- You'll benefit from flexible pressure sensors embedded in wound dressings that instantly alert caregivers to potential complications
- Your treatment will utilize placental tissue applications that promote faster cell growth and create effective allografts
- You'll see AI-driven imaging tools that automatically measure and classify wounds with unprecedented accuracy
- Your care will include wearable sensors providing real-time evaluation of healing parameters, ensuring thorough wound management at every stage
Frequently Asked Questions
Can Therapy Rays Be Used on Infected Wounds That Have Already Been Bandaged?
You shouldn't apply therapy rays to bandaged infected wounds. You'll need to remove the bandage first for proper assessment and treatment. Instead, focus on appropriate wound care and antibiotics for managing infections.
How Long Should Patients Wait Between Multiple Therapy Ray Treatment Sessions?
You'll need to consult your healthcare provider for specific timing between therapy ray sessions, as there's no universal standard. They'll determine intervals based on your wound type, infection severity, and treatment response.
Do Therapy Rays Work Effectively on Wounds Exposed to Water or Sweat?
Yes, therapy rays can work effectively on your moist or wet wounds. You'll just need water-resistant patches and proper dressings. Lower irradiance levels maintain effectiveness while staying safe in wet conditions during treatment.
Can Patients Receive Therapy Ray Treatments While Taking Oral Antibiotics?
You can receive therapy ray treatments while taking oral antibiotics, as there's no known direct contraindication. They work differently – rays target bacteria locally while antibiotics work systemically through your bloodstream.
Are There Specific Wound Types Where Therapy Rays Should Not Be Used?
You shouldn't use therapy rays on burns, recent injuries, wounds with cancer, or areas with metal implants. If you've had recent surgery or have fever, it's best to avoid therapy rays completely.
In Summary
You'll find therapy rays are revolutionizing wound care by targeting harmful bacteria while preserving healthy tissue. With proven success against drug-resistant strains, these treatments offer a safer alternative to traditional antibiotics. Whether you're dealing with chronic wounds or acute injuries, light therapy's early detection capabilities and diverse applications make it a game-changing tool. Watch for more breakthroughs as this technology continues transforming wound management protocols.





Leave a Reply