Phototherapy accelerates your wound healing through seven proven mechanisms. It stimulates your mitochondria to produce more energy for cellular repair while triggering critical healing pathways. You'll experience increased collagen production as fibroblasts become more active, strengthening damaged tissue. The therapy reduces inflammation by converting harmful inflammatory cells into healing-focused ones. It boosts blood vessel formation, delivering essential nutrients to wounds. Light exposure speeds up cell division for faster wound closure and activates pain-relieving responses. For stubborn wounds, specific wavelengths target multiple healing processes simultaneously. Understanding these mechanisms can transform your approach to wound recovery.
The Science Behind Light Healing

The science of phototherapy represents a fascinating intersection of physics and biology. When specific wavelengths of light penetrate your tissue, they trigger a complex cascade of cellular events that promote healing.
At the heart of this process is your cells' power plant – the mitochondria – where light activates the Cytochrome C complex, boosting ATP production and energizing cellular repair.
You'll find it's not heat that creates these healing effects, but rather non-thermal photochemical reactions. The light specifically activates endogenous proteins like TGF-beta 1, which controls how your cells grow and divide. This therapy has been proven particularly effective in treating third-degree burns through controlled laser protocols. Research has shown that the 658 nm wavelength is particularly effective, outperforming other wavelengths in stimulating tissue repair and promoting new blood vessel formation.
NASA's research has validated these findings, demonstrating that near-infrared light can accelerate wound healing, especially in oxygen-starved tissues. While different wavelengths show varying degrees of effectiveness, they all work through similar cellular mechanisms.
Your body responds to therapeutic doses of light by reducing inflammation and increasing collagen production, essential steps in the wound healing process.
Collagen Production and Tissue Repair
Light therapy's stimulation of fibroblast growth pathways triggers a remarkable cascade of healing events in your damaged tissue.
As these specialized cells multiply, they're producing increased amounts of type-1 collagen, which forms the essential building blocks for wound repair. Studies show that exposure to 660nm deep red light significantly boosts this collagen production process.
This enhanced collagen synthesis leads directly to stronger tissue matrix rebuilding, where new proteins create a framework for complete wound closure.
Stimulating Fibroblast Growth Pathways
Three key mechanisms drive phototherapy's effect on fibroblast growth pathways: FGF stimulation, Ras/MAPK pathway activation, and enhanced collagen production.
Photobiomodulation (PBM) directly stimulates the release of Fibroblast Growth Factor, a vital cytokine that's often deficient in diabetic wounds. This process works through the activation of the Ras/MAPK signaling pathway, which promotes cell growth and survival.
When you use LED phototherapy, you're triggering a cascade of cellular responses. The light interacts with your tissues to activate the Ras/MAPK pathway, which then enhances cell proliferation and differentiation. This activation is particularly important because it leads to increased collagen synthesis and improved tissue repair.
You'll see multiple benefits from this process: enhanced angiogenesis, reduced inflammation, and accelerated healing rates. While experimental studies show stronger evidence than clinical trials, LED phototherapy has proven effective in treating chronic wounds, especially in diabetic patients.
The treatment's success depends on specific parameters like wavelength and energy density, but it's becoming increasingly preferred over LASER therapy due to its cost-effectiveness and ease of use.
Light-Enhanced Collagen Synthesis
Photobiomodulation's impact on collagen synthesis represents a pivotal advancement in wound healing therapy. When specific wavelengths of light penetrate your skin, they trigger a cascade of cellular events that boost your body's natural healing mechanisms.
The process works through light energy's interaction with your cells' mitochondria, increasing ATP production and activating fibroblasts – the cells responsible for collagen synthesis. Studies show that maintaining proper fluence of 3-6 J/cm² is crucial for optimal therapeutic outcomes.
You'll find that dual-wavelength therapy, combining 635 nm and 830 nm light, offers enhanced benefits by targeting multiple photoacceptor molecules simultaneously.
Key benefits of phototherapy for collagen production include:
- Accelerated wound closure through increased collagen synthesis
- Enhanced tissue strength and integrity during healing
- Improved fibroblast activation and proliferation
- Reduced inflammation in the wound area
- Increased formation of new blood vessels (angiogenesis)
Research demonstrates that near-infrared laser light at 830 nm particularly excels at stimulating human skin fibroblasts. When combined with LED therapy, you'll experience faster tissue repair and more efficient wound healing.
This scientifically-proven approach has revolutionized wound management by harnessing light's natural ability to boost your body's collagen production capabilities.
Tissue Matrix Rebuilding Process
Building upon the fundamentals of collagen synthesis, the tissue matrix rebuilding process represents a complex interplay of cellular activities that work together to restore damaged tissue.
When you undergo phototherapy, light wavelengths between 600-1000nm trigger a cascade of healing responses in your body's tissue matrix. Type III collagen gradually converts to stronger type I collagen during the healing process.
The process works through multiple mechanisms: first, the light stimulates your fibroblasts to produce more collagen, particularly at 660nm wavelengths. You'll see enhanced tissue repair as phototherapy promotes fibroblastic proliferation and increases blood vessel formation. The therapy also reduces inflammation and oxidative stress, which speeds up wound closure.
You'll experience healing benefits across different phases. During the inflammatory phase, phototherapy reduces swelling and oxidative damage. In the proliferative phase, it stimulates new cell growth and capillary formation. The maturation phase benefits from improved collagen cross-linking and better scar remodeling.
For ideal results, you'll need specific therapeutic parameters. The effectiveness depends on precise wavelengths, dosages, and application duration. When combined with conventional treatments, LED phototherapy substantially improves your healing outcomes, especially for challenging wounds like diabetic ulcers.
Fighting Inflammation Through Light

You'll notice remarkable reductions in inflammatory cells when using phototherapy for wound healing, as specific wavelengths of light target and modulate the body's inflammatory response.
Light therapy strengthens your free radical defense system while reducing oxidative stress, creating an ideal environment for tissue repair. Studies show that treatments using 410-430 nm wavelengths deliver optimal healing results.
Your wound's healing response accelerates through this process, as the light helps convert pro-inflammatory M1 macrophages to healing-focused M2 macrophages, marking a faster shift to the recovery phase.
Light Reduces Inflammatory Cells
Light therapy triggers a powerful cascade of anti-inflammatory effects within wounded tissue, making it a promising treatment for accelerating healing. When light reaches your cells, it stimulates chromophores in mitochondria and activates calcium ion channels, boosting ATP production and cellular energy.
This process initiates a series of biological responses that directly combat inflammation and promote healing.
Your body's inflammatory cells respond to light therapy in several remarkable ways:
- Light stimulates fibroblasts to increase collagen production, essential for wound repair
- It generates reactive oxygen species that fight harmful microorganisms
- It decreases inflammatory markers in activated macrophages
- It reduces pro-inflammatory cytokines like IL-1β and IL-18
- It boosts anti-inflammatory cytokines such as IL-10
Clinical evidence supports these effects, showing that wounds treated with phototherapy display improved healing markers. You'll see better re-epithelialization, decreased inflammation, and increased blood vessel formation in treated areas.
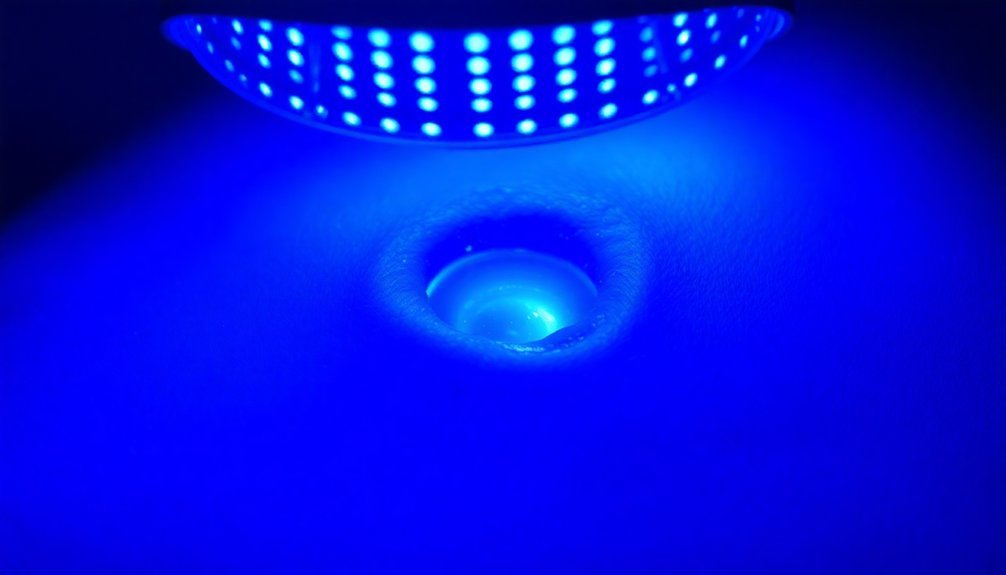
While researchers are still working to establish standardized protocols, they've found that different wavelengths of light, particularly blue light, can effectively reduce wound size and accelerate recovery through these anti-inflammatory mechanisms.
Free Radical Defense System
The body's natural defense system against free radicals gets a powerful boost from photobiomodulation (PBM) therapy. When red and near-infrared light penetrate your skin, they trigger antioxidant defenses that protect you from cellular damage and premature aging. This therapy enhances your cells' ability to fight oxidative stress and return to a balanced state. A healthy diet rich in whole food antioxidants can further enhance these protective effects.
PBM works on multiple levels to combat inflammation. It strengthens your mitochondrial membranes, improves oxygen intake, and increases ATP production, all while modulating cytokine expression. The therapy effectively reduces pro-inflammatory cytokines while boosting anti-inflammatory ones like IL-10, giving you extensive protection against inflammation.
When you're exposed to red light therapy, your keratinocytes respond by decreasing TNF-α expression and pro-inflammatory cytokine secretion. The treatment activates your MAPK pathway in a way that suppresses inflammatory markers like IL-6 and IL-8. Studies consistently show that this process helps restore normal cytokine levels, particularly in conditions like atopic dermatitis.
Through these mechanisms, PBM not only protects your cells but also actively promotes healing and tissue repair.
Accelerated Healing Response
Through precisely targeted wavelengths, photobiomodulation therapy accelerates your body's natural healing response in multiple ways. When specific red and near-infrared light wavelengths penetrate your tissues, they trigger a cascade of healing mechanisms that dramatically speed up recovery. Research shows that TGF-beta 1 protein becomes activated during photobiomodulation, helping regulate cell growth and division.
Your cells respond by producing more ATP, reducing inflammation, and increasing blood flow to damaged areas.
The healing acceleration becomes particularly evident at the 633nm wavelength, where you'll experience enhanced tissue repair and reduced scarring. Your body's wound healing can improve by up to 19 days compared to untreated areas.
Here's how photobiomodulation boosts your healing response:
- Stimulates platelet activation and aggregation, speeding up cell migration
- Increases production of collagen and essential growth factors
- Reduces inflammatory markers and controls pain signaling
- Improves blood flow to damaged tissues
- Decreases reactive oxygen species in stressed cells
For the best results, you'll typically need treatments three times per week at specific wavelengths and energy densities. While 633nm works well for general wound healing, your healthcare provider might recommend different wavelengths based on your specific condition and wound type.
Enhanced Blood Vessel Formation
Phototherapy's impact on blood vessel formation represents a significant breakthrough in wound healing treatments. When you're exposed to specific wavelengths of light, particularly 660 nm laser therapy, your body responds by creating new blood vessels and expanding existing ones. This enhanced blood vessel formation, or angiogenesis, is essential for delivering oxygen and nutrients to healing tissues.
Both laser and LED treatments can effectively stimulate blood vessel growth. You'll see superior results with light doses between 1-5 J/cm², with 4 J/cm² being particularly effective for activating collagen formation.
| Light Type | Wavelength | Primary Benefits |
|---|---|---|
| Red Laser | 660 nm | Superior vessel formation |
| Green LED | 530 ± 20 nm | Increased angiogenesis |
| Red LED | 700 ± 20 nm | Enhanced wound healing |
When combined with bioengineered scaffolds, you'll experience even better results. These scaffolds, loaded with endothelial cells, work synergistically with phototherapy to accelerate healing. The combination therapy improves re-epithelialization and vascularization, particularly beneficial for treating deep burn wounds. You'll notice the most significant improvements during the proliferation phase, with measurable progress tracked from day 1 through day 35.
Accelerated Cell Growth

Three key cellular processes drive accelerated wound healing during phototherapy: increased collagen production, enhanced cell division, and heightened fibroblast activity. When you undergo light therapy, particularly at the 660 nm wavelength, your cells respond by ramping up collagen Type 1 production, which is essential for wound repair and tissue regeneration.
The ideal dosage of 4 J/cm² triggers accelerated cellular responses that promote faster healing. You'll benefit from light therapy's ability to stimulate your body's natural healing mechanisms through photobiomodulation, which directly impacts cell division and tissue repair.
Here's what happens at the cellular level during phototherapy:
- Your fibroblasts become more active, producing more collagen
- Cell division accelerates, leading to faster wound closure
- New tissue formation increases through enhanced cellular proliferation
- Collagen synthesis ramps up, especially with red light exposure
- Granulation tissue develops more rapidly
Your skin's absorption of specific light wavelengths, particularly in the red and near-infrared ranges, activates these cellular processes. This scientific approach to wound healing isn't just theoretical – it's backed by both laboratory studies and clinical evidence showing measurable improvements in healing rates.
Pain Management With Light
Beyond accelerating cell growth, light therapy offers remarkable pain management benefits during wound recovery. When specific wavelengths of light penetrate your tissue, they trigger the release of TGF-beta 1, which helps control inflammation and cellular repair. The therapy reduces oxidative stress and supports your body's natural healing responses.
You'll experience reduced pain as the therapy enhances blood flow to wounded areas while activating healing cells like fibroblasts and macrophages.
Clinical evidence shows you can expect significant pain reduction across various wound types. Whether you're dealing with surgical incisions, diabetic ulcers, or burn injuries, light therapy effectively manages both acute and chronic pain without the side effects of traditional medications. It's particularly effective for challenging conditions like venous ulcers and cancer-related oral mucositis.
You'll find this treatment especially valuable if you're looking for a non-invasive pain management solution. The therapy works by modulating your cells' oxidative states and boosting cellular energy production, which naturally reduces inflammation.
Research consistently demonstrates that this approach not only decreases your pain levels but also speeds up the healing process, making it a reliable option for both immediate pain relief and long-term recovery.
Healing Resistant Wounds
Managing resistant wounds presents unique challenges that light therapy effectively addresses through multiple healing mechanisms. When you're dealing with stubborn wounds that won't heal through conventional treatments, phototherapy offers a scientifically-proven solution that works at the cellular level.
The most effective approach combines specific wavelengths with ideal treatment protocols. You'll find that 633 nm light shows particularly promising results for diabetic wounds, while blue light (410 nm) helps control bacterial infections. For the best outcomes, treatments using 4 J/cm² have proven more effective than lower doses.
Here's how phototherapy tackles resistant wounds:
- Boosts cellular function and migration, speeding up the healing process
- Increases collagen production, especially with 660 nm wavelength exposure
- Enhances mitochondrial activity, leading to higher ATP production
- Controls antibiotic-resistant bacteria through blue light therapy
- Reduces inflammation while protecting diabetic cells
You can expect the best results with consistent treatment sessions every other day for a week. When combined with photosensitizers like methylene blue, you'll see even better outcomes, particularly in cases involving antibiotic-resistant infections.
Frequently Asked Questions
Can Phototherapy Treatments Be Done at Home Without Professional Supervision?
You can safely use phototherapy at home for minor wounds with FDA-approved devices, but you'll need proper training and should consult healthcare providers first, especially for severe wounds requiring professional supervision.
How Long Does a Typical Phototherapy Session Last?
Your typical phototherapy session will last 15-30 minutes, but it'll vary based on your treatment type. UVB sessions can be just seconds long, while UVA treatments might take up to an hour.
Are There Any Side Effects or Risks Associated With LED Phototherapy?
Yes, you'll need to watch for potential side effects like burning, redness, swelling, and skin rashes. It's important to avoid sun exposure after treatment and always wear protective gear during your sessions.
Can Phototherapy Be Used During Pregnancy for Wound Healing?
Yes, you can safely use phototherapy during pregnancy for wound healing. It's non-invasive and studies show no significant adverse effects. It's particularly helpful for C-section recovery, though you should consult your healthcare provider first.
How Many Phototherapy Sessions Are Typically Needed to See Results?
You'll typically notice improvements after 6-8 sessions, but full results may require 15-25 treatments. For wound healing specifically, you'll need 6-12 sessions, with each session lasting a few minutes to 30 minutes.
In Summary
You'll find phototherapy to be a groundbreaking advancement in wound healing, backed by solid scientific evidence. Whether you're dealing with chronic wounds or seeking faster recovery, light therapy offers multiple pathways to healing through collagen stimulation, inflammation reduction, and improved circulation. By understanding these proven benefits, you can make informed decisions about incorporating phototherapy into your wound care routine.





Leave a Reply