Low-frequency ultrasound devices have revolutionized wound healing in 2025, with clinical studies showing up to 40% faster recovery times. You'll find these portable devices particularly effective as they use 20 kHz frequencies to stimulate tissue repair and increase blood flow naturally. The latest wearable models, like Drexel University's watch-sized device, deliver precise acoustic energy directly to your wound site, promoting cell growth and reducing inflammation in just 3-20 minute sessions. Built-in AI monitoring and smart sensors track your healing progress in real-time, while clinical trials demonstrate six times higher healing rates than traditional methods. The transformative potential of this technology is just beginning to unfold.
Current State of Wound Care
Three major trends are revolutionizing modern wound care: artificial intelligence, smart devices, and advanced imaging technologies.
AI-driven solutions are transforming how healthcare providers assess and treat wounds, using big data to support clinical decisions and create personalized treatment plans. AI systems can now analyze 3D mobile images of wounds, providing accurate measurements and actionable insights with higher precision than traditional methods. The market for these innovative technologies is experiencing remarkable growth, with projections showing a compound annual growth of 5.08% through 2032.
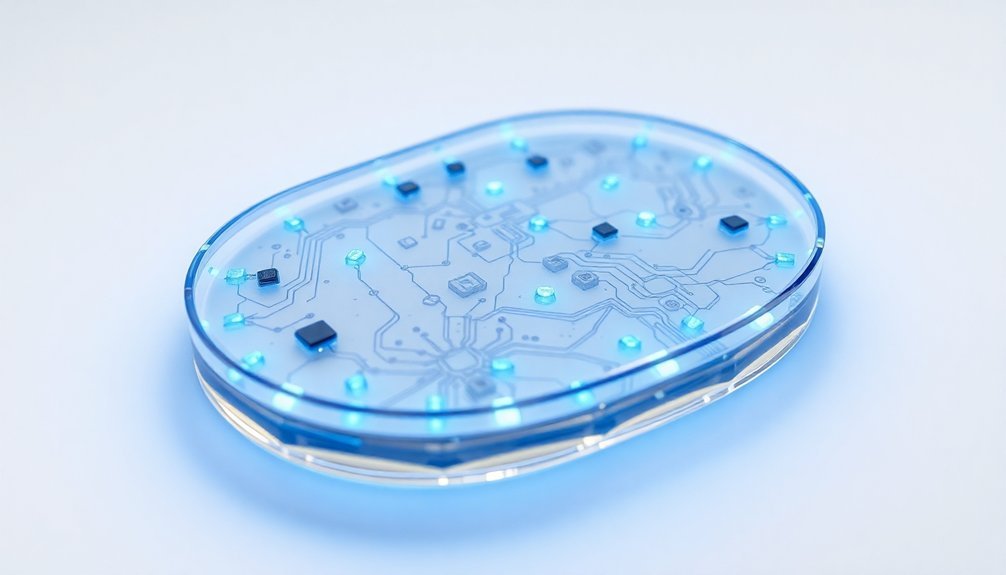
Smart devices have become essential tools in wound management. You can now access wearable sensors that deliver real-time feedback, while smart bandages monitor healing progress and automatically dispense medications as needed. These devices communicate with your healthcare team, alerting them to any concerning changes in your wound status.
The integration of advanced imaging technologies has improved wound assessment accuracy substantially. You'll benefit from fluorescent and thermal imaging techniques that detect issues before they're visible to the naked eye.
Digital imaging technologies, combined with AI-powered analysis, now outperform human experts in predicting wound healing outcomes. These innovations guarantee you receive more precise, data-driven care while reducing the risk of complications.
Understanding Ultrasound Healing Technology
When you use ultrasound for wound healing, high-frequency sound waves create mechanical vibrations that stimulate tissue repair and increase blood flow to the affected area.
During treatment, ultrasound therapy helps prevent infection risks by targeting wounds early in the healing process.
You'll find that ultrasound devices operate at specific energy levels designed to promote healing while maintaining safety, typically delivering treatments in 3-20 minute sessions depending on the wound size.
The technology reduces inflammation and bacteria in the wound bed while triggering your body's natural healing response at the cellular level, making it an effective non-invasive treatment option.
How Ultrasound Promotes Healing
Several remarkable mechanisms make ultrasound therapy one of today's most effective wound healing technologies. When ultrasonic waves penetrate your tissue, they trigger a cascade of healing responses at the cellular level. Studies demonstrate that patients treated with ultrasound therapy achieve 50% faster healing by week 12.
You'll find that these waves enhance cell growth and promote the migration of epithelial cells, which are essential for wound closure and protection.
The healing process accelerates as ultrasound therapy:
- Stimulates fibroblast activity, organizing collagen for better tissue strength
- Increases blood flow to the wound site, delivering necessary nutrients and oxygen
- Reduces inflammation naturally, helping you experience less pain and discomfort
- Promotes the development of myofibroblasts, which minimize scarring
You'll benefit from ultrasound's ability to speed up wound healing through multiple phases. During the inflammatory phase, it shortens the acute response time, while in the proliferative phase, it boosts tissue strength and encourages wound contraction.
What's particularly impressive is that you won't experience any discomfort during treatment, as it's completely non-invasive. Research consistently shows that ultrasound therapy can prevent chronic wound development and reduce your risk of requiring surgery.
Energy Levels and Safety
Understanding the right energy levels and safety protocols is critical for effective ultrasound wound therapy.
You'll find that energy levels diminish exponentially as ultrasound waves penetrate deeper into tissues, with more absorption occurring in superficial layers. The half-value depth, which varies by tissue type and frequency, tells you how deep the energy can effectively reach. For optimal treatment outcomes, ultrasound frequency of 3MHz is recommended for dermal wounds.
When you're selecting treatment parameters, you'll need to take into account that higher frequencies have shorter penetration depths but may be more effective for superficial wounds. Different tissues absorb ultrasound energy at varying rates, which directly affects your treatment's success. You'll want to carefully monitor therapeutic dosages to prevent tissue damage while maintaining effectiveness.
Safety considerations must be your top priority. The ultrasound's acoustic streaming affects cell membrane permeability, and high-intensity applications can cause concerning thermal effects.
You'll need to verify proper equipment maintenance and receive adequate training before administering treatments. To maximize safety and effectiveness, you should:
- Monitor treatment intensity and duration
- Check equipment calibration regularly
- Understand tissue-specific absorption rates
- Follow established safety protocols
- Maintain proper documentation of treatments
Clinical Research and Evidence

Clinical research has stepped up to validate the effectiveness of modern wound healing devices through extensive studies and trials. The data shows remarkable outcomes, particularly with TWO2 therapy demonstrating six times higher healing rates and substantially lower recurrence compared to standard care within 12 months. The therapy achieves 82% healing success in diabetic foot ulcers within 56 days of treatment.
Real-world evidence and randomized controlled trials support these findings, while innovative technologies like the CELLADEEP patch have shown impressive results in accelerating wound closure.
You'll find that clinical studies are actively monitoring both traditional and emerging treatment methods, with ultrasound therapy showing a 15% increase in weekly healing rates.
- TWO2 therapy patients are 6 times more likely to heal within 12 weeks compared to standard care
- CELLADEEP patch studies reveal enhanced fibroblast activity and improved skin parameters
- Low-frequency ultrasound devices demonstrate measurable improvements in healing rates
- Near-infrared diagnostic monitoring effectively tracks blood vessel growth and oxygenation
Interdisciplinary collaboration between biomedical engineering, medicine, and nursing continues to drive innovation in wound healing research, while ongoing clinical trials evaluate the safety and efficacy of new devices, ensuring evidence-based advancement in treatment options.
Device Specifications and Features
Modern wound healing devices pack powerful features into increasingly compact and user-friendly designs. You'll find advanced systems like the WoundEL device, measuring just 190 x 130 x 45 mm and weighing 600g, making it highly portable for continuous treatment during daily activities. The device uses 128 Hz frequency as its default setting for optimal wound healing stimulation.
These devices offer customizable settings to match your specific wound care needs. NPWT systems like WoundPro deliver adjustable negative pressure up to -200 mmHg, while electric stimulation devices provide pre-set therapy sessions of 30 minutes with automatic shutoff features.
You're protected by built-in safety systems, including alarms that alert you to vacuum leaks, blockages, or low battery conditions.
The latest models come equipped with real-time monitoring capabilities, letting your healthcare provider track your wound's progress and make data-driven adjustments to your treatment plan.
You'll also benefit from versatile dressing options, including both hydrophobic and hydrophilic foam dressings in various sizes. Battery-powered operation guarantees you're not tethered to a power outlet, while detailed user manuals and professional oversight help you achieve ideal results from your chosen device.
Treatment Protocols and Applications

When using advanced wound healing devices, you'll need to follow specific application protocols that align with standard treatment guidelines and the device manufacturer's instructions.
You must adhere to prescribed treatment durations, which typically range from 4-16 weeks depending on wound type and healing progress, while documenting weekly measurements and treatment responses.
To guarantee maximum safety and effectiveness, you'll need to maintain proper device parameters, including pressure settings for negative pressure therapy or intensity levels for ultrasound treatments, while monitoring the wound site for any adverse reactions. For effective outcomes in diabetic foot ulcers, implementing early detection strategies is critical to prevent complications and reduce healing time.
Application Methods and Setup
The proper setup and application of wound healing devices sets the foundation for successful treatment outcomes. When implementing Negative Pressure Wound Therapy (NPWT), you'll need to start with thorough wound evaluation and sterilization using alcoholic chlorhexidine.
After debriding any infected tissue, apply a non-paraffinized polyester net before sealing with specialized adhesive dressing. Stage III and IV pressure ulcers, along with arterial, diabetic, and venous stasis ulcers are approved for electrical stimulation treatment coverage.
For electrical stimulation treatments, you'll work with wearable nanogenerators that convert breathing energy into power for AC circuits. These devices deliver precise microcurrents that mimic your body's natural electrical signals, promoting faster healing and reducing pain through controlled stimulation.
- Apply 3D-bioprinted dressings using smart bandages with programmable therapeutic delivery
- Position stem cell-based biopolymers directly onto the wound surface using products like ReGenerCell™
- Set up electrical stimulation devices by placing electrodes strategically around the wound area
- Install NPWT systems by confirming proper seal and connection to the vacuum source
Each application method requires careful attention to detail and sterile technique. For 3D-bioprinted solutions, you'll need to confirm proper matrix placement for ideal tissue regeneration, while stem cell-based treatments require precise cellular distribution for maximum effectiveness.
Treatment Duration Guidelines
Successful wound healing requires carefully planned treatment durations that vary substantially based on wound type and severity. You'll need to understand that hard-to-heal wounds, which show less than 50% area reduction after 4 weeks, may require extended NPWT treatment periods lasting several months.
For the best results, you should change NPWT dressings every 48-72 hours, though infected wounds might need more frequent changes. If you're dealing with non-infected wounds, plan for at least three changes per week.
Don't let therapy interruptions exceed 2 hours, as you'll need to change the dressing if they do.
You'll find that NPWT effectiveness varies among patients and wound types. Both traditional electric and portable battery-powered devices have shown promising results in reducing infection rates. However, you must remember that not all wounds respond equally to this treatment.
Consider your patient's age, smoking status, and overall health when determining treatment duration. You'll need to avoid using NPWT on exposed blood vessels and follow your institution's guidelines for pressure settings.
Regular assessments will help you adjust the treatment plan as needed.
Device Safety Parameters
Maintaining strict safety parameters stands at the forefront of effective wound healing device protocols. You'll need to guarantee your wound healing devices meet rigorous sterilization standards, with validated terminal sterilization methods like gamma radiation or ethylene oxide.
When selecting devices, particularly for Negative Pressure Wound Therapy (NPWT), it's vital to verify they include essential safety features and comply with regulatory requirements for their device classification.
For maximum safety in wound healing applications, you should prioritize these critical parameters:
- Verify the device's Sterility Assurance Level (SAL) and biocompatibility testing documentation according to ISO-10993 standards
- Confirm built-in safety features like pressure control mechanisms, filters, and alarm systems for NPWT devices
- Check for contraindications specific to your patient's condition, especially with necrotic tissue or untreated osteomyelitis
- Guarantee proper validation methods and shelf-life testing are documented for all device components
Your device selection should account for material compatibility with other medical equipment and include clear documentation of sterilization methods. Remember that regular monitoring and adherence to specified pressure ranges are essential for preventing complications and ensuring ideal healing outcomes.
Safety and Effectiveness Data
Safety monitoring and effectiveness validation remain central pillars in wound healing device development, with regulatory bodies like the FDA implementing stricter oversight measures. You'll need to understand that wound-healing products now require either Premarket Approvals (PMAs) or 510(k) clearances, depending on their antimicrobial resistance risk levels.
| Device Type | Safety Requirements | Effectiveness Metrics |
|---|---|---|
| Smart Bandages | Real-time monitoring | Healing rate tracking |
| NPWT Systems | Infection control | Tissue granulation |
| Natural Compounds | Biocompatibility tests | Collagen formation |
When you're evaluating wound healing devices, you'll find that advanced technologies like bioelectronic materials and smart hydrogels offer enhanced monitoring capabilities. Machine learning tools now play a vital role in analyzing wound healing data, while standardized assessment criteria guarantee reliable evaluations. You'll notice that successful devices often combine multiple approaches, from microRNA-based biopolymers to negative pressure therapy. The effectiveness of these devices is continuously monitored through postmarket surveillance, ensuring they maintain their therapeutic benefits while meeting strict safety standards.
Cost-Benefit Analysis

When evaluating wound healing devices, you'll need to weigh their substantial upfront costs against their long-term benefits. The projected market growth to USD 21.15 billion by 2030 reflects healthcare providers' recognition that investing in advanced wound closure technologies can lead to considerable cost savings over time.
You'll find the most cost-effective solutions in the disposable NPWT devices segment, which is expected to reach USD 529.7 million by 2034. These devices deliver impressive results while helping you manage operational costs effectively.
Consider these key financial factors when selecting wound healing devices:
- Initial investment vs. reduced treatment duration – advanced devices may cost more upfront but can accelerate healing time
- Disposable vs. conventional options – disposable NPWT devices offer lower maintenance costs and reduced risk of cross-contamination
- Staff training requirements – simpler devices may require less training time and associated costs
- Complication rates – devices with lower complication rates can markedly reduce follow-up treatment expenses
As healthcare costs continue rising, you'll want to focus on solutions that combine therapeutic effectiveness with economic efficiency. The shift toward disposable devices particularly demonstrates how innovation can align with cost-effectiveness in wound care management.
The shift toward disposable devices particularly demonstrates how innovation can align with cost-effectiveness in wound care management.
Patient Success Stories
Real success stories from wound care centers shine a light on the transformative power of modern healing devices. At Grand Lake Health System, several patients have experienced remarkable recoveries using advanced treatment options. Donna's condition improved markedly with Hyperbaric Oxygen Therapy (HBOT) after other treatments failed, while David achieved complete leg healing through surgical intervention and specialized care.
The success stories don't stop there. Carolyn V.'s wounds closed successfully using Vacuum Assisted Closure (VAC) therapy, and Virginia K.'s leg was saved through a combination of HBOT and surgical procedures.
These outcomes demonstrate how modern devices can make a critical difference in patient recovery.
Successful wound healing often involves a combination of cutting-edge technology and personalized care. Patients consistently report high satisfaction levels, particularly when receiving thorough treatment plans that include advanced devices like HBOT chambers, VAC systems, and innovative dressings.
The key to these success stories lies in the integration of appropriate healing devices with expert medical care, resulting in improved healing rates and better quality of life for patients with complex wounds.
Future Developments and Innovations

The future of wound healing stands at the forefront of medical innovation, with breakthroughs in stem cell therapy, 3D printing, and AI-driven solutions transforming patient care.
You'll see mesenchymal stem cells revolutionizing treatment by differentiating into skin cells and promoting blood vessel formation, while smart bandages with integrated sensors will monitor your healing in real-time.
Advanced technologies are merging to create personalized solutions you couldn't have imagined a decade ago. 3D printing now enables custom skin grafts, while AI analyzes millions of wound cases to determine the most effective treatment for your specific condition.
- Bioactive wound dressings using your own cells will provide a rich environment of growth factors, accelerating healing
- Wearable nanogenerators will power portable electrical stimulation devices, making treatment more convenient
- Gene therapy treatments will enhance your body's natural healing abilities by correcting defective genes
- AI-powered imaging systems will track your wound healing progress and automatically adjust treatment plans
These innovations aren't just theoretical – they're backed by clinical trials and market projections showing substantial growth through 2030, making advanced wound care more accessible and effective than ever before.
Frequently Asked Questions
Can the Device Be Used While Swimming or Showering?
Yes, you can safely swim and shower with these waterproof dressings. They'll stay securely in place, creating a reliable barrier that keeps water out while letting your wound breathe through microscopic channels.
How Long Does the Battery Last Before Needing Replacement?
Your device's battery life varies, but you'll typically get 14+ hours of use. You'll need to recharge or replace batteries depending on your specific model, with most requiring attention every 1-2 days.
Will Insurance Companies Cover the Cost of This Treatment?
Your insurance may cover treatment if you have diabetic foot ulcers or venous leg ulcers that haven't improved after four weeks of standard care. You'll need to pay a $257 deductible and 20% copayment.
Can Multiple Devices Be Used Simultaneously on Different Wound Sites?
Yes, you can use multiple wound healing devices simultaneously on different wound sites. However, you'll need to consult your healthcare provider to guarantee proper coordination and safety of combined treatments for ideal healing outcomes.
Are There Any Dietary Restrictions While Using the Ultrasound Device?
You don't need to follow any specific dietary restrictions while using ultrasound therapy. However, maintaining a healthy, balanced diet rich in protein, vitamins, and minerals will help support your wound healing process naturally.
In Summary
You'll find low-frequency ultrasound devices leading the future of wound healing technology. These compact, wearable solutions offer promising results for faster recovery times and improved patient outcomes. With ongoing research and development, you can expect to see more innovative features and wider accessibility by 2025. When choosing a wound healing device, consider the clinical evidence, cost-effectiveness, and your specific healing needs.





Leave a Reply